
In healthcare, nothing is quite as effective as a personal touchpoint. A phone call from a real human – to schedule your follow-up appointment, check in on your symptoms, remind you to test your blood sugar, or coordinate a referral to a physical therapist – makes a far greater impact than an impersonal text, email, or robocall. And in a world where health systems increasingly rely on reimbursements from value-based contracts, these phone calls can significantly affect the system's bottom lines.
But getting and staying in touch with your thousands of patients is no small task. Your staff has to track touchpoints and keep track of the patients that need to be called back. The data has to be manually spliced together and distributed to managers and call agents. The result is often a folder of messy and complicated spreadsheets – difficult to merge, subject to high levels of human error, and nearly impossible to use for regular reporting.
Why Every System Needs Outbound Calling
The days of fee-for-service aren’t over… yet. However, more and more healthcare payers are pushing providers into risk-based contracts to promote value-based care. In 2020, payments tied to alternative payment methodologies increased nearly 25 percent from five years prior.1
Whether it’s through the Medicare Quality Payment Program (Medicare QPP), commercial insurers, or state Medicaid agencies, these trends will only continue to accelerate. At the same time, fee-for-service remains healthcare’s bread and butter. Driving appointment volume for necessary visits, referrals, and follow-up care continues to be critical. Leveraging outbound calling for appointment reminders, follow-up care coordination, and outreach can drive visits and revenue to your system.
Millions Of Dollars Are On The Line
Your highest risk patients need your services, your reminders, your touchpoints. Activating them is the difference between bringing in millions in quality bonuses and losing money in reimbursement when you fail to meet – or measure – your performance goals.

Medicare Advantage has paid out over $47.5 billion in quality payments since 2015. Average per enrollee quality payouts for traditional Medicare and commercially insured patients can range from $278 to $521.2 Revenue for quality incentives adds up quickly and is not something most systems are willing to leave on the line.
Focus On The Phone Call
Calling patients directly is more effective than text, email, or mail. It allows healthcare staff to make a direct, personalized connection with a patient. It also allows the patient to ask questions, make changes to an appointment, update information like insurance or contact details, and more.
The data supports what we already know intuitively. For example, making direct calls increased the uptake of health insurance by 22.5 percent in a recent Covered California campaign.3
But overworked staff, long patient lists, messy spreadsheets, and increasing reporting requirements make a cohesive, outbound calling strategy a major challenge. Healthcare systems need a simple, effective way to use outbound calling to activate their highest-risk patients and report on the results of those calls. That’s why Actium Health’s outbound calling capability boosts a call center’s efficiency and helps them prove out their success.
Five Ways Actium Health’s Outbound Calling Management Can Get You Ready For Success In 2023
- Happier patients with personal, targeted phone calls. Suffice it to say, the past few years have been a whirlwind for the healthcare industry. Patients are relying on your help to navigate an arena that’s been devastated by the pandemic and turned upside down by workforce shortages, telehealth, and constantly changing policies. Patient satisfaction is a critical component of everything your health system does. Friendly, targeted, personal phone calls – calls where your patients have the opportunity to talk to staff, ask questions, and make any necessary changes – is a major boost to patient satisfaction.
- Happier and more productive staff. Messy spreadsheets, rife with human error, greeting you when you login to your computer in the morning is not an ideal way to work. Staff need a clean, sophisticated interface they can use to track phone calls and view updates. This leads to less time spent sorting through someone else’s work. Moreover, managers can easily view progress, seamlessly pulling aggregate metrics to measure and report on outbound calling productivity.
- Better outcomes for the highest risk patients. Using outbound calling for care management has a direct impact on your patients’ health. One study looked at telephone care management for diabetes patients at a VA hospital. It found that the patients were more likely to self-monitor, get a cholesterol test, be seen in a specialty clinic, and more.4 Outbound calls can help you find success on a range of HEDIS and QPP measures like comprehensive diabetes care, controlling high blood pressure, HbA1c control, postpartum follow-up care, and hospital 30-day readmissions.
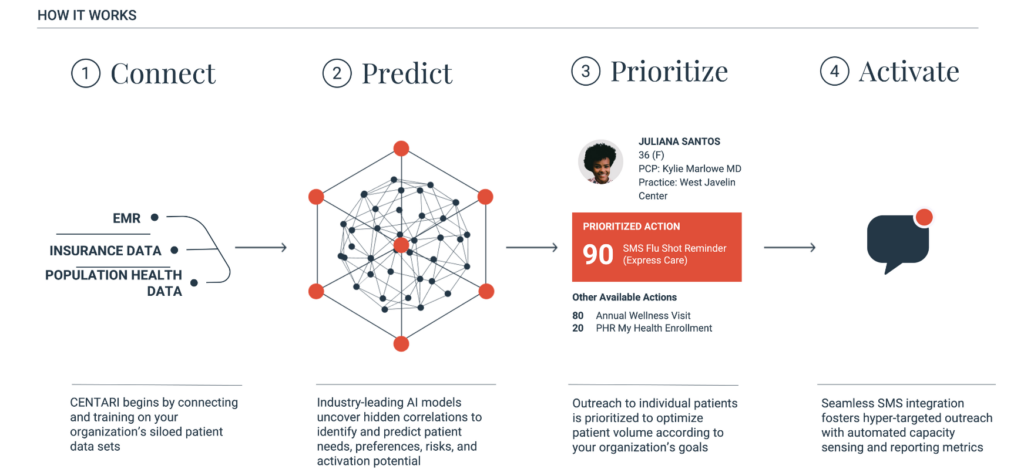
The best part? Actium Health can help you prioritize your patient list. By integrating with your EHR, population health management tool, and other sources of patient data, Actium Health can prioritize your outreach. It uses artificial intelligence to predict level of risk and likelihood of engagement. That way your staff always begins with the patients most in need of care – and the ones that are most likely to engage. - Measurable progress through sophisticated reporting capabilities. Healthcare payers are increasingly requiring reports on care management, population health, and quality improvement. And healthcare managers are looking to demonstrate the value of their outreach efforts on the system’s bottom line.
Actium Health’s outbound calling interface streamlines reporting by tracking which patients received a phone call and who called them. Moreover, it will track the result of the phone call – whether an appointment was made, or whether a follow-up call is needed. Leaders can provide reports on call volume by staff as well as call outcomes over time. Then they can directly tie those call outcomes to quality metrics for their high-risk patients, effortlessly demonstrating their ROI. - Increased risk-based reimbursements in the areas you need it most. As value-based payment arrangements continue to proliferate, healthcare systems still need to fill their empty appointment slots with their highest-risk patients. This is where Actium Health comes in. First, it can leverage your existing patient data to determine which patients would benefit most from a particular service. This could be cardiovascular services, diabetes management, nutrition, primary care, and more. Then, using outbound calling, staff can easily track calls to those patients, coordinating their appointments to further their goals – goals like boosting quality metrics, filling care gaps, increasing medication and care plan compliance, and more.
Finally, Actium Health’s dynamic throttling capability means you never have to worry about overbooking. The platform merges with your provider schedules so that you only reach out to patients to book services when there is availability in the schedule.
Steps To A Successful Outbound Calling Program
- Touch base with the Actium Health team by requesting a demo. Let them know you’re interested in perfecting your outbound calling. They can set you up with a demo of our outbound calling and reporting services.
- Actium Health will sort through your various sources of patient data. It integrates with your EHR, population health management tool, and other patient data sources.
- Then, Actium Health will use these patient data sources to develop a prioritized patient contact list, sorted based on your key business priorities. The campaign could be driving service to your new primary care clinic, checking in on your high-risk diabetes patients, or following up on your maternity patients postpartum.
- With their own unique logins, call agents can directly access their assigned outbound campaigns from the outbound calling feature. The patients will be available to call in priority order, with the option to filter on a subset of patients based on urgent business priorities. For example, an agent can focus only on patients on a particular insurance plan, or near a specified clinic location.
- As calls are made, the outcome of each interaction will be logged and automatically updated with a timestamp and the name of the agent that completed the call. Freeform notes on the interaction can be recorded, if needed, and available for the next agent to view before calling that patient.
- The platform syncs in real-time, so there is no need to worry about overlapping calls. Multiple staff can make calls, take notes, and track results from all of your locations.
- Actium Health makes it easy to track follow-up calls. Patients that require a follow-up will automatically pop into the queue at the requested date and time. If the agent who connected with them most recently is not available, the patient will be connected to the next available outbound calling agent. This way it's easy to close the loop, no one slips through the cracks, and patients have confidence that their health system values providing consistent, positive experiences.
- Management can easily pull sophisticated, presentation-ready reports in seconds. A call center manager can pull agent-level, operational metrics like calls made, answer rate, etc. by campaign, to identify their best performers, capacity, and areas for improvement. Stakeholders can also see the direct results of those calls including appointments scheduled, encounters completed, and other downstream results driven directly by the outbound calling team.
You need a way to activate your highest-risk patients efficiently and effectively to make sure you drive visits, close care gaps, boost quality metrics, and bring in revenue for your system. Doing so is critical to success not only for value-based care but also to maximize fee-for-service reimbursements with appointment volume. Actium Health’s outbound calling feature can help you achieve all of this, tracking your productivity and outcomes driven by outbound calls.
Interested in learning more? Touch base with the Actium Health team today.

Sources:
1 Health Care Payment Learning & Action Network, 2021 LAN APM Measurement Effort, available at: https://hcp-lan.org/apm-measurement-effort/2020-2021-apm/#1638982499890-78a9577c-d60c
2 The Commonwealth Fund, Taking Stock of Medicare Advantage, Quality Reporting and Quality Bonuses. Available at: https://www.commonwealthfund.org/blog/2022/taking-stock-medicare-advantage-quality-reporting-and-quality-bonuses and KFF, Spending on Medicare Advantage Quality Bonus Program Payment Reached $10 Billion in 2022. Available at: https://www.kff.org/medicare/issue-brief/spending-on-medicare-advantage-quality-bonus-program-payment-reached-10-billion-in-2022/
3 Myerson, et al. Personalized Telephone Outreach Increased Health Insurance Take-Up For Hard-To-Reach Populations, But Challenges Remain. Health Affairs. Available at: https://www.healthaffairs.org/doi/10.1377/hlthaff.2021.01000
4 Piete, et al. Impact of Automated Calls With Nurse Follow-Up on Diabetes Treatment Outcomes in a Department of Veterans Affairs Health Care System: A randomized controlled trial. Diabetes Care. Available at: https://diabetesjournals.org/care/article/24/2/202/24152/Impact-of-Automated-Calls-With-Nurse-Follow-Up-on

