
Q&A with Brad Kittredge
Founder and CEO
Brightside Health
COVID-19 forced countless patients and providers to transition from face-to-face health care to virtual care and telemedicine. But virtual care has the potential to go far beyond increasing access to care. It can harness data to deliver more effective treatment and improve health outcomes.
Brad Kittredge is the CEO and Co-Founder at Brightside Health, a virtual behavioral health platform designed to increase access and improve outcomes for patients with depression and anxiety. In the following Q&A, Brad discusses how Brightside is transforming delivery of behavioral health care and what the implications are for treatment of other chronic conditions.
Tell us about yourself and why you started Brightside Health.
Brad: I co-founded Brightside Health with Jeremy Barth and Dr. Mimi Winsberg in 2017. Our mission is to deliver measurably better virtual behavioral health outcomes at scale. Telemedicine is a great tool to expand access to care, but there are still systemic quality issues in mental health care. If we simply move care online, we're going to help more people get access to subpar care. Instead, we have the opportunity to use a new set of resources to deliver better care to more and more people.
The existing system has treated mental health as one condition and made the assumption that everybody has similar needs. The reality is that it's a highly heterogeneous condition with varied patient needs. For us, that’s a motivator to do better.
How does Brightside Health deliver personalized virtual behavioral health care?
Brad: One of the huge challenges that has held back mental health care for decades is the lack of outcomes measurement. Until recently, it was estimated that fewer than 10 percent of mental health practitioners were practicing measurement-based care. We were spending tens of billions of dollars on mental health without knowing whether it was working.
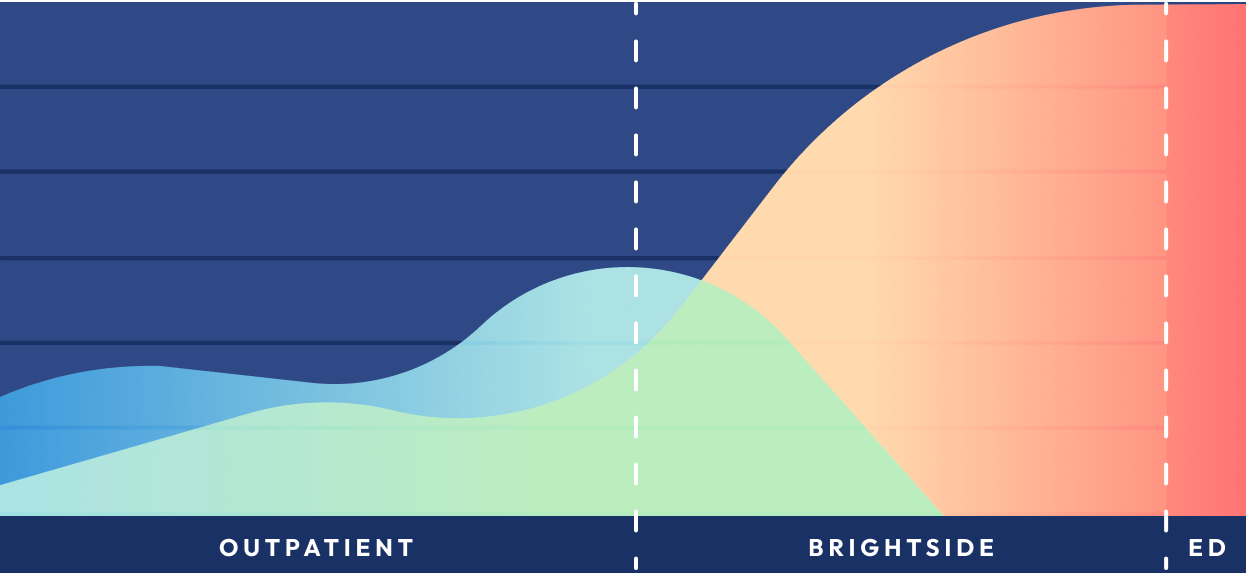
Once we have outcomes data, we have to use it to deliver timely interventions. Our health care system, and the mental health system in particular, often gives every patient the same pathway: "Try this and come back to see me in six weeks and tell me how you're doing." We know that people have very different pathways, and our ability to measure and monitor remotely allows us to intervene on a more timely basis.
We then have to inform the right intervention for the patient. We use clinical decision support, analyzing data relative to published research, clinical best practices, as well as data within our own population to make data-driven recommendations to providers. That way they can prescribe the right medication for an individual's unique needs.
Finally, we have to get the patient experience right so that the patient is in the driver’s seat. We want patients to have great alliances with their providers as well as clarity on how to drive better behavioral health outcomes for themselves.
How is virtual care challenging the status quo?
Brad: Many people assumed there was a trade-off with telemedicine. They assumed that you would increase convenience, but then quality of care would suffer. We didn't like that assumption. Actually, we thought that by delivering care via telemedicine we could deliver better care.
There is a health system in the Midwest that's consistently considered one of the best of the health systems in the country. We compared our outcomes data against theirs and found that we had 50 percent higher treatment response and remission rates than the system.
With telemedicine, we have a new set of tools to question certain clinical approaches and standards of care. We have an opportunity to deliver not just more convenient care, but better virtual behavioral health care.
Can mental health care in particular benefit from telemedicine?
Brad: Behavioral health has been the leading use case for telemedicine – around half of telemedicine claims have been for behavioral health encounters. It’s a leading use case that can help us to figure out what's working and not working.
Especially for chronic conditions, it’s important to have a one-to-one patient-provider relationship rather than a pool of providers. This helps to develop an effective therapeutic alliance for decision-making. And patients not only don't have to drive to the doctor's office, but they can have more frequent touchpoints.
Providers practicing in a remote care environment have more control over the way they practice. They have more direct and ongoing relationships with their patients. At Brightside, we've invested in the tools that providers use to minimize time spent on administrative or billing work, allowing them to focus on clinical care.
What are key considerations for quality assurance in virtual behavioral health care?
Brad: We have to make sure that there is consistent adherence to evidence-based care and clinical best practices across a group of providers. Traditionally, care supervision involves curbside consults or second opinions and random chart reviews. With digital care, we can do quality assurance on every case. The system can look at every chart for completeness, medication interactions, and other things that can trigger proactive supervision.
How are payers responding to new virtual care models?
Brad: Many payers have leaned into telemedicine adoption. They see it as an opportunity to improve care availability as well as data capture and reporting. In virtual behavioral health, I see the convergence of telemedicine adoption and value-based care because we have data. We know whether care is actually working for an individual and across a patient population, which unblocks the main barrier to value-based payment.
How do you effectively engage patients in their care?
Brad: In mental health in particular, treatment adherence is really low. The proportion of people who fill their first prescription for an antidepressant is small, and then a lot of people experience side effects or fail to improve. It's really important, particularly in the early stages of treatment, to engage people and on-board them into their care.

To start, we have to make people feel like they're in the right place. For example, we don't call our members “patients”. “Members” are a part of a group focused on helping to manage the mental health challenges in their lives. For so long, healthcare was opaque to the patient. The doctor had all the information and made decisions in a silo. All the data we capture, and all the information we have, we share with the patient. That way members can see their progress, understand when they have setbacks, and have informed conversations with their providers.
Then, we have to remove any barriers to care. When we launched our native app, we saw really good penetration and engagement because it removed barriers like logins and used push notifications to trigger actions. We've also been investing in adding a lot of people to our data team. We use predictive models to identify when somebody might become non-adherent, and we can identify people who have a predictive behavioral footprint that might give us reason to intervene proactively. It’s a great use case for machine learning.
Are patients resistant to receiving virtual behavioral health services?
Brad: In our experience, when people are struggling with mental health challenges, they know it. Everybody wants to feel better, but it has been hard to access mental health care. In these cases we have to extend a hand and engage people in a respectful way that gives them hope and keeps it simple. Providing easy stepping stones to care has been very effective for us.
How do you measure success in virtual behavioral health?
Brad: The way we measure success depends on the audience. For Brightside, success begins and ends with clinical outcomes and our ability to measurably improve people's lives.
For the consumer, priority number one is feeling better. All of our providers get compassionate and culturally responsive care training, because we want every patient to feel heard, valued, and supported throughout their care.
When we're working with our payer partners, we focus on clinical outcomes as well as demonstrating the return on investment so they understand the value of certain programs and continue to invest in those programs.
What best practices from virtual behavioral health can be replicated in other areas of health care?
Brad: Brightside was the first to go to market with a consumer medication management solution for mental health. A lot of people weren’t sure whether it could be done remotely – whether consumers would like it and whether it would be safe and clinically effective. We did a lot of analysis and felt strongly that medication management in mental health could be done remotely, and we have shown that to be the case.
The same process is occurring for every chronic condition. People are asking, "Can we really do this remotely?" Mental health has an advantage in that you don’t generally need a physical exam to appropriately assess and treat someone. Still, we are seeing lots of thoughtful approaches to providing remote care as well as finding hybrid models of care that might be driven virtually.
It's all got to start with data. Everything needs to be measured so that you can trigger interventions, measure outcomes, and, of course, measure return on investment.
One of the advantages of a digital platform is that it can institute clinical guidelines. Telemedicine is so much more than web visits. There is an opportunity to use technology, data, and clinicians to deliver the right care for the right patient at the right time, driven by what the evidence and data show to be most effective. A lot of cool stuff is happening in cardiac health, diabetes care, and other areas. People are taking lessons from digital health and applying them across chronic conditions.
Listen to the full Hello Healthcare podcast interview with Brad on your preferred streaming platform, or listen to the recording below.
About Brad Kittredge
As the CEO and co-founder of Brightside Health, Brad works to increase access to mental health care with measurably better outcomes. He has spent over a decade pioneering evidence-based and healthcare solutions for companies like Jawbone and 23andMe. Find Brad Kittredge on LinkedIn.

